Tear Duct Problems and Tear Duct Surgery
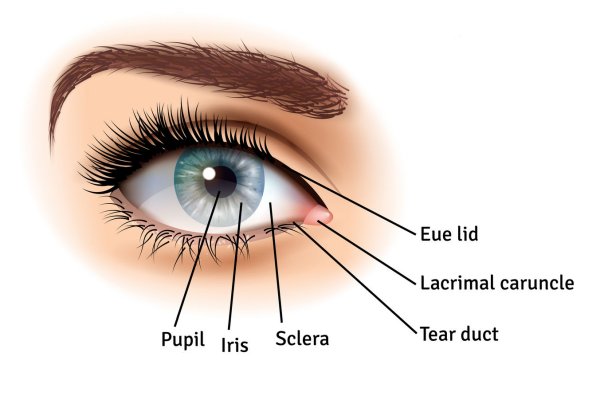
When tear ducts are working correctly, tears that are released from the lacrimal glands (on the outer side of each eye) pass across the surface of the eye, draining through holes in the eyelids and into the lacrimal sac on each side of the nose. From here, the tears empty into the nose via the nasolacrimal, or tear duct.
A tear duct blockage prevents tears from draining into the nose and causes pooling of tears, with watery eyes, irritation and painful swelling.
What causes a blocked tear duct?
Babies commonly suffer blocked tear ducts due to incomplete opening of the distal end of tear duct in the nose. Adults often develop a blocked tear duct due to tear duct infection or injury. In older adults, a blocked tear duct is often caused by a narrowing of the tear drainage system.
Here are some causes of a blocked tear duct:
- Chronic sinus infections
- Scar tissue from an injury such as a broken nose
- Narrowing of the puncta (the opening of the tear ducts in the eyelid) through age
- Conjunctivitis and other infections
- Nasal polyps
- Abnormalities, such as a deviated nasal septum
What are the symptoms of a blocked tear duct?
There are a number of symptoms that can be a sign of a blocked tear duct:
Watery eyes, or tears overflowing
Irritated eyes
Mucus discharge, or dried discharge around the eye
Blurry vision
Regular eye infections
Swelling near the eyes, on one side of the nose
How is a blocked tear duct treated?
Babies that are born with a blocked tear duct do not usually need any treatment and the condition will improve within 4-5 months. 90-95% of children with blocked tear ducts will settle after 18-24 months with minor treatment, which may include:
Lacrimal sac massage – this is massaging the inside corner of your child’s eyelids 2-3 times a day, or as directed by a doctor.
Local lid hygiene management – this involves cleaning any discharge with a warm washcloth and antibiotic eye drops if the discharge becomes excessive.
In 5-10% of paediatric cases, a surgical intervention with syringing and probing of tear ducts is required after the child turns 2 years old. If this method is unsuccessful and the tear duct continues to block, we would proceed to surgical treatment involving placing stents into the tear duct, for 2-3 months before then removing them.
In adults, treatment is usually required, the form of which depends on the cause of the obstruction.
For mild cases, the treatment includes:
Cleaning the eyelids
Warm compresses
Prescription ointment to reduce swelling
For more severe cases:
In severe cases, a surgical procedure known as a dacryocystorhinostomy is used. This surgery creates a new passage between the nose and lacrimal sac which bypasses the blockage. The Surgeon places stents in this passage to keep it open while it heals. This procedure is highly successful in 90% of cases.
In other cases, the Surgeon may decide to build a new drainage system using a procedure called conjunctivodacryocystorhinostomy.
If the blockage is caused by a tumour, it is most likely that we recommend the tumour is shrunk or removed before any other treatments are carried out.
Tear duct problems caused by blocked or narrowing puncta (tear entry holes in the eyelids) are treated by widening the entry holes or puncta through dilation, probing and irrigation treatments.
If your tear duct blockage is caused by scarring or chronic inflammation, a procedure called balloon catheter dilation is carried out to open or widen the passages.
Aftercare
After surgery, you will need to use a nasal decongestant and eyedrops to reduce inflammation and prevent infection. You will receive follow-up appointments as required, and if stents have been used, these will be removed after 3-6 months.
Please get in touch for a consultation to discuss further treatment and your tear duct surgery.